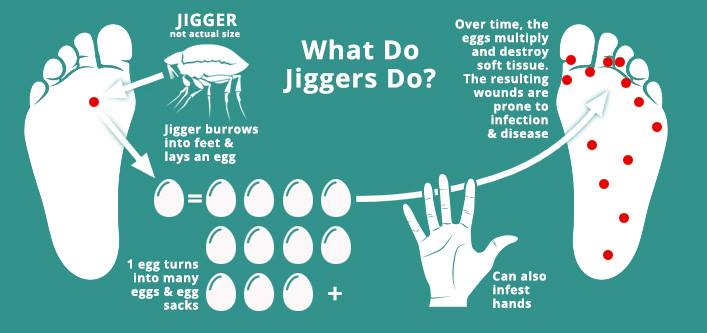
What comes to your mind when you think of jiggers? For those who might perhaps have seen its effects, an ick would be the perfect response. A disclaimer that the images might be highly graphical for some readers. They are tiny parasitic fleas that burrow into one’s skin causing painful and itchy lesions. Tunga penetrans- its Latinized name- often affects people living off-grid in rural areas with sandy soil.
As of 2022, Kenya’s Ministry of Health had projected that nearly 10 million citizens were at risk of being infected. Jiggers are also called Tungiasis. According to the World Health Organization, nearly one billion people globally live in areas suitable for its transmission. They have stated that no country conducts surveillance on these fleas so the real number is unknown. They mostly occur in tropical and subtropical regions of the Caribbean, South America and sub-Saharan Africa.
Tungiasis is diagnosed through visual examination, with live fleas presenting as whitish discs of varying sizes, featuring a dark centre that darkens over time as the flea dies, ultimately turning black. In areas where Tungiasis is common, individuals, including children, often recognize their infection. Many attempt to remove the fleas themselves, resulting in distinctive circular lesions with the remnants of the dead flea, indicating recent infection. The morbidity associated with Tungiasis, both acute and chronic, stems from the inflammatory response around the embedded female sand fleas, which can worsen due to bacterial superinfection. During the acute phase, symptoms include redness, swelling, peeling, pain, and itching, with scratching increasing the likelihood of bacterial complications. Large abscesses may develop as a result. While the feet are the most frequently affected area, infestation can occur elsewhere on the body. Bullous lesions have also been observed. Chronic consequences include fissures, ulcers, lymphangitis,
lymphoedema, ascending neuritis, nail loss, and tissue necrosis. These complications lead to pain, functional impairment, disfigurement, and alterations in gait for those suffering from
Tungiasis.

The parasitic infection caused by sand fleas primarily affects individuals living in extreme poverty. This socioeconomic factor encourages behaviors that elevate the risk of infection, such as residing in homes with unsealed earthen floors, infrequent washing of feet, and the absence of soap during personal hygiene routines. Additionally, in certain communities, the presence of infected dogs or pigs is associated with increased rates of infection. To achieve a long-lasting decline in both the incidence of Tungiasis and its related health issues, a One Health approach is essential. This strategy should incorporate behavior modifications aimed at enhancing soap usage for daily foot washing, applying insecticides to floors or sealing them, addressing infections in animal populations, and providing treatment for affected humans. The consistent application of a coconut oil-based repellent has shown effectiveness in preventing flea penetration into the skin. When this repellent is used on the feet twice daily, the morbidity associated with Tungiasis decreases sharply, nearing zero within 8 to 10 weeks. Even with intermittent use, the reduction in morbidity is substantial, showcasing the importance of preventive measures in controlling this infection.
In regions where sand fleas are endemic, the mechanical extraction of these burrowed parasites often occurs as a desperate measure. Typically, this procedure is performed by the affected individuals or their caregivers using non-sterile tools such as sticks, hairpins, thorns, safety pins, sewing needles, or scissors. This painful process can be particularly traumatic for children and may lead to local inflammation if the parasite ruptures, potentially introducing pathogenic bacteria and resulting in a secondary infection. Additionally, the instruments are frequently reused on multiple patients, posing a risk for disease transmission, including hepatitis B virus (HBV), hepatitis C virus (HCV), and HIV. To ensure safety, mechanical extraction should be conducted exclusively with surgical instruments by a trained nurse under sterile conditions. Post-extraction, it is crucial to properly dress the wound and verify the patient’s tetanus vaccination status, administering a booster if necessary. For effective and safe treatment, topical applications of a formulation containing two low-viscosity dimethicone oils (NYDA®) are recommended. In Kenya, various initiatives have been implemented to address the jigger problem. A notable example is the local campaign led by Catherine Omanyo in Busia County, which aims to assist over a thousand families by promoting hygiene, providing fumigation resources, and increasing awareness of the issue. This initiative underscores the significance of anti-jigger treatments in schools, where infestation rates are particularly high due to insufficient infrastructure and sanitation facilities.
Community-driven solutions, such as the Dabaso Tujengane program, have demonstrated effectiveness by utilizing locally available neem and coconut oils to manage jigger infestations
and ensure clean household environments. These efforts significantly improve conditions for affected children, allowing them to return to school.
Raising awareness and tackling the stigma associated with jiggers are crucial steps toward enhancing health outcomes and fostering preventive measures in Kenya. Sustainable approaches,
including consistent household fumigation, education on hygiene practices, and collaboration with health partners, are vital for the long-term eradication of jiggers and to garner community support in regions impacted by this issue.

